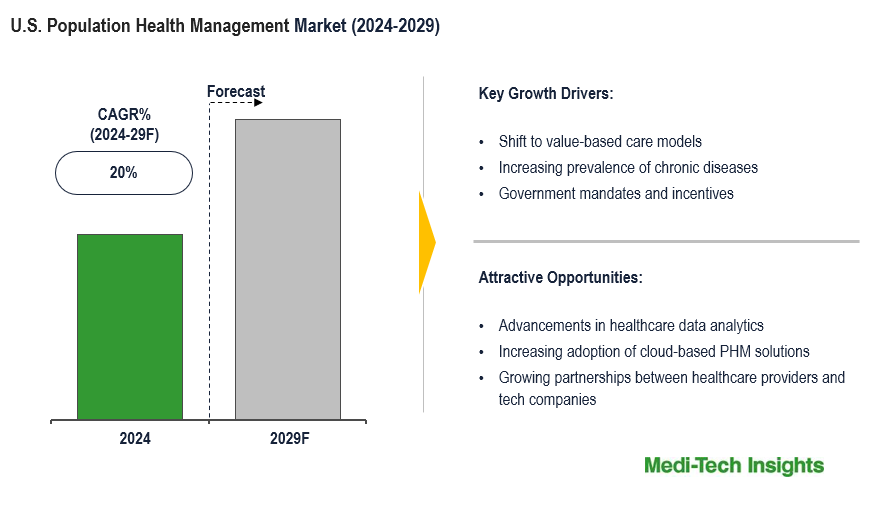
U.S. Population Health Management (PHM) Market Size, Share, and Demand 2024 to 2029 is expected to grow at a CAGR of 20% by 2029.
The U.S. population health management market is expected to grow at a significant CAGR of approximately 20% in the forecast period. This growth is driven by the transition to value-based care models, the increasing burden of chronic diseases, advancements in healthcare analytics, regulatory reforms, and the rising need for cost reduction and improved care outcomes. However, barriers such as high implementation costs and concerns over data privacy pose challenges to wider adoption. To learn more about the research report, download a sample report.
Report Overview
The U.S. population health management (PHM) market focuses on improving health outcomes for defined populations by using various tools, including healthcare data analytics, care coordination, and patient engagement strategies. Its goal is to enhance the quality of care, reduce healthcare costs, and improve patient satisfaction by shifting from reactive care to preventive and proactive interventions. PHM typically involves collaboration between healthcare providers, payers, and public health entities to manage chronic diseases, reduce hospital admissions, and achieve value-based care outcomes.
To learn more about this report, download the PDF brochure
Emphasis on Value-Based Care Models: Driving Market Demand
A significant factor driving the demand for population health management is the growing shift from traditional fee-for-service models to value-based care. Value-based care focuses on improving patient outcomes and reducing costs through better care coordination, preventive care, and chronic disease management. This model incentivizes healthcare providers to prioritize long-term health and cost efficiency, aligning perfectly with the objectives of PHM. As healthcare systems aim to reduce hospital readmissions and lower overall costs, PHM strategies, supported by data-driven approaches, have become indispensable. The success of this shift depends on real-time data sharing, care integration, and collaborative decision-making, making PHM tools central to achieving these goals.
Market Trend: Rise of AI and Machine Learning in Population Health Management
One of the most transformative trends in the U.S. population health management market is the integration of AI and machine learning technologies. AI-driven analytics allow for the processing of vast amounts of healthcare data, providing insights that help predict patient risks, tailor treatment plans, and enhance care coordination. These technologies enable healthcare providers to identify high-risk patients early, automate repetitive tasks, and optimize population-level interventions. By leveraging AI, healthcare organizations can not only improve the accuracy of diagnoses and treatments but also deliver more personalized, efficient care, ultimately driving better health outcomes while reducing operational costs. The ability to predict health trends and deliver targeted preventive care is rapidly becoming a key advantage in PHM initiatives.
To learn more about this report, download the PDF brochure
Competitive Landscape Analysis
The U.S. population health management market is marked by the presence of established and emerging market players such as Cerner Corporation (Oracle); Veradigm LLC (Allscripts Healthcare, LLC); eClinicalWorks; Conifer Health Solutions, LLC; Cedar Gate Technologies (Enli Health Intelligence); McKesson Corporation; Medecision; Optum, Inc.; Koninklijke Philips N.V.; and Athenahealth, Inc. among others. Some of the key strategies adopted by market players include product innovation and development, strategic partnerships and collaborations.
Report Scope
| Report Scope | Details |
| Base Year Considered | 2023 |
| Historical Data | 2022 - 2023 |
| Forecast Period | 2024 - 2029 |
| Growth Rate | CAGR of 20% |
| Market Drivers |
|
| Attractive Opportunities |
|
| Segment Scope | Product, Mode of Delivery, End User |
| Regional Scope | U.S. |
| Key Companies Mapped | Cerner Corporation (Oracle); Veradigm LLC (Allscripts Healthcare, LLC); eClinicalWorks; Conifer Health Solutions, LLC; Cedar Gate Technologies (Enli Health Intelligence); McKesson Corporation; Medecision; Optum, Inc.; Koninklijke Philips N.V.; and Athenahealth, Inc. among others. |
| Report Highlights | Market Size & Forecast, Growth Drivers & Restraints, Trends, Competitive Analysis |
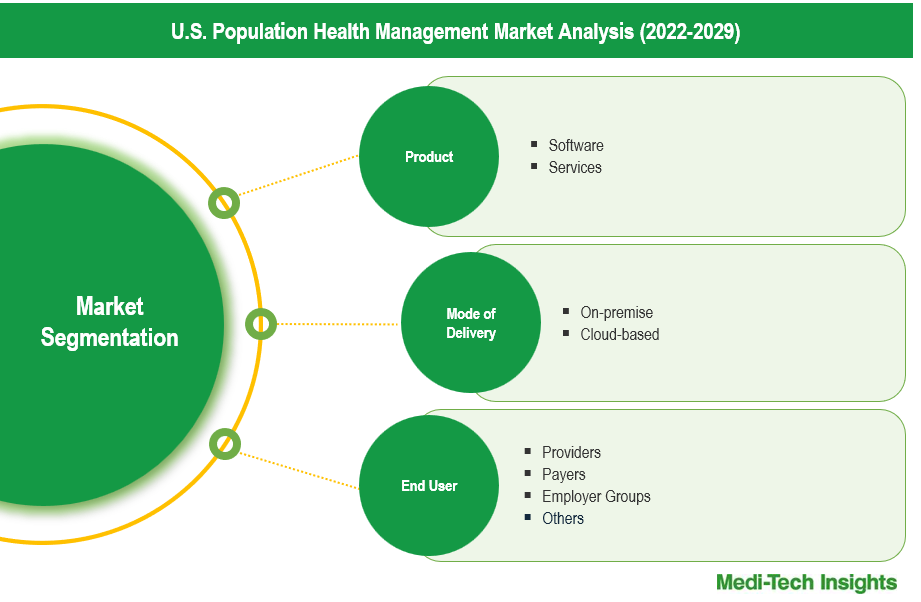
Market Segmentation
This report by Medi-Tech Insights provides size of the U.S. population health management (PHM) at a regional level from 2022 to 2029. The report further segments the market on the basis of product, mode of delivery, and end user.
- Market Size & Forecast (2022-2029), By Product, USD Million
- Software
- Services
- Market Size & Forecast (2022-2029), By Mode of Delivery, USD Million
- On-premise
- Cloud-based
- Market Size & Forecast (2022-2029), By End User, USD Million
- Providers
- Payers
- Employer Groups
- Others
Key Strategic Questions Addressed
-
What is the market size & forecast of the U.S. population health management market?
-
What are historical, present, and forecasted market shares and growth rates of various segments and sub-segments of the U.S. population health management market?
-
What are the key trends defining the market?
-
What are the major factors impacting the market?
-
What are the opportunities prevailing in the market?
-
Who are the major players operating in the market?
-
What are the key strategies adopted by players?
- Introduction
- Introduction
- Market Scope
- Market Definition
- Segments Covered
- Research Timeframe
- Currency Considered
- Study Limitations
- Stakeholders
- List of Abbreviations
- Key Conferences and Events (2023-2024)
- Research Methodology
- Secondary Research
- Primary Research
- Market Estimation
- Bottom-Up Approach
- Top-Down Approach
- Market Forecasting
- Executive Summary
- S. Population Health Management (PHM) Market Snapshot (2023-2029)
- Segment Overview
- Competitive Insights
- Market Overview
- Market Dynamics
- Drivers
- Shift to value-based care models
- Increasing prevalence of chronic diseases
- Government mandates and incentives
- Growing focus on preventive care
- Rising demand for cost-effective healthcare solutions
- Restraints
- High implementation and maintenance costs
- Data privacy and security concerns
- Lack of standardized data exchange formats
- Opportunities
- Advancements in healthcare data analytics
- Increasing adoption of cloud-based PHM solutions
- Key Market Trends
- Adoption of AI-driven predictive analytics
- Rising use of patient engagement tools and mobile health apps
- Unmet Market Needs
- Industry Speaks
- Regulatory Analysis
- Drivers
- Market Dynamics
- S. Population Health Management Market Size & Forecast (2022-2029), By Product, USD Million
- Introduction
- Software
- Services
- S. Population Health Management Market Size & Forecast (2022-2029), By Mode of Delivery, USD Million
- Introduction
- On-premise
- Cloud-based
- S. Population Health Management Market Size & Forecast (2022-2029), By End User, USD Million
- Introduction
- Providers
- Payers
- Employer Groups
- Others
- Competitive Landscape
- Key Players and their Competitive Positioning
- Key Player Comparison
- Segment-wise Player Mapping
- Market Share Analysis (2023)
- Company Categorization Matrix
- Dominants/Leaders
- New Entrants
- Emerging Players
- Innovative Players
- Key Strategies Assessment, By Player (2022-2024)
- New Product Launches
- Partnerships, Agreements, & Collaborations
- Mergers & Acquisitions
- Geographic Expansion
- Key Players and their Competitive Positioning
- Company Profiles*
(Business Overview, Financial Performance**, Products Offered, Recent Developments)
- Cerner Corporation (Oracle)
- Veradigm LLC (Allscripts Healthcare, LLC)
- eClinicalWorks
- Conifer Health Solutions, LLC
- Cedar Gate Technologies (Enli Health Intelligence)
- McKesson Corporation
- Medecision
- Optum, Inc.
- Koninklijke Philips N.V.
- Athenahealth, Inc
- Other Prominent Players
The study has been compiled based on extensive primary and secondary research.
Secondary Research (Indicative List)

Primary Research
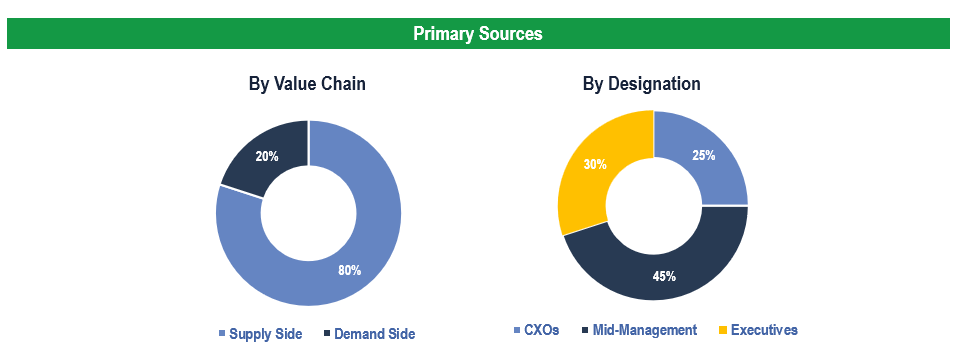
To validate research findings (market size & forecasts, market segmentation, market dynamics, competitive landscape, key industry trends, etc.), extensive primary interviews were conducted with both supply and demand-side stakeholders.
Supply Side Stakeholders:
- Senior Management Level: CEOs, Presidents, Vice-Presidents, Directors, Chief Technology Officers, Chief Commercial Officers
- Mid-Management Level: Product Managers, Sales Managers, Brand Managers, R&D Managers, Business Development Managers, Consultants
Demand Side Stakeholders:
- Providers, Payers, Employer Groups and Others
Breakdown of Primary Interviews
Market Size Estimation
Both ‘Top-Down & Bottom-Up Approaches’ were used to derive market size estimates and forecasts
Data Triangulation
Research findings derived through secondary sources & internal analysis was validated with Primary Interviews, Internal Knowledge Repository and Company’s Sales Data